Enter your email to receive the CareQuest newsletter:
Medical-Dental Integration
The link between oral health and systemic health — between the mouth and the body — are increasingly clear. And to treat the whole person, our health system needs to recognize these connections and bridge the silos between medical care and dental care.
The Connection Between Oral Health and Overall Health
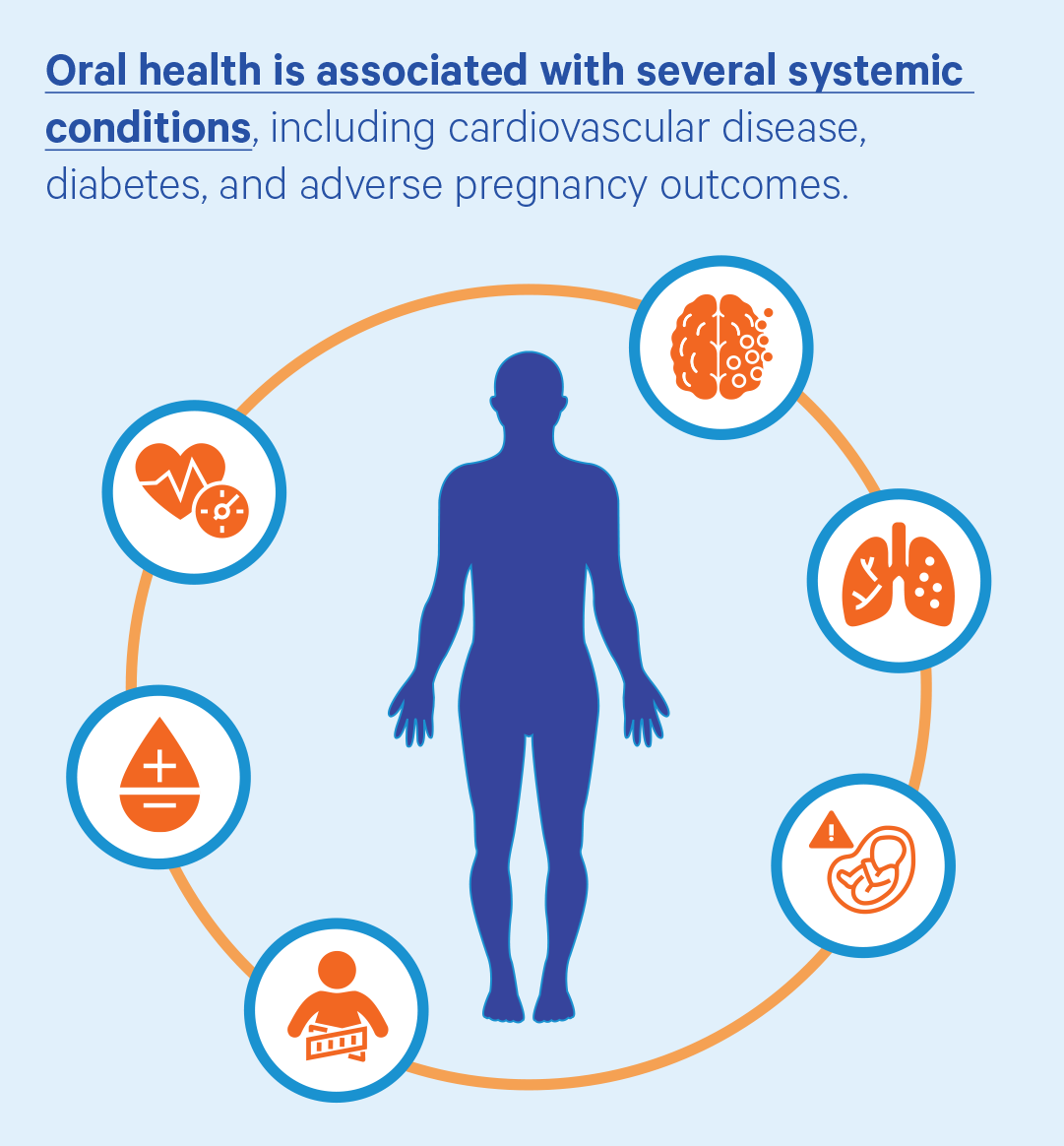
Oral health problems can contribute to a variety of other health problems, including high blood pressure, difficulty managing diabetes, risk of developing Alzheimer’s disease, and pregnancy complications. Good oral health practices and preventive dental care, on the other hand, can benefit overall health. Oral health and overall health are connected. But despite the growing understanding of the relationship between oral health and systemic disease, oral health care often remains siloed from the rest of the health care system.
Medical-dental integration can help build that critical bridge between oral health and overall health. It’s an approach to care that integrates dental medicine into primary care and behavioral health. It also promotes the practice of dental providers integrating services such as screenings for chronic diseases into their care. It is a model of care that encourages providers to come up with comprehensive care plans for the whole person.
Medical-Dental Integration in Action
Medical Oral Expanded Care (MORE Care™)


Community Oral Health Transformation (COrHT)


Dental Data Exchange Project


The Value of Medical-Dental Integration
Medical-dental integration can improve the care experience for patients and reduce costs at the same time. In addition to the $520 million Medicare spends annually on dental emergency department visits, the exacerbation of other conditions means increased expenditures and negative outcomes in other areas of health care, as well. If these issues were caught and managed early, many of those expenditures could be avoided.
Ensuring Care for the Most Vulnerable
Medical-dental integration has also been an important strategy for increasing access to care for vulnerable populations. As patients visit their primary care office for medical treatment, for example, there’s an opportunity for primary care providers to address oral health by assessing oral health risk and reinforcing at-home care messaging, creating an access point for patients who might not otherwise seek dental care.
86%
92%
95%
$520M
Recent Progress Toward Integration
Many community health programs and Federally Qualified Health Centers (FQHCs) are already working toward medical-dental integration. These collaborative approaches educate patients about the connections between oral health and overall health, promoting prevention behaviors and strategies. In addition, some dentists are providing screenings for chronic diseases such as diabetes, high blood pressure, and cholesterol. These services have been shown to provide substantial cost savings to health systems as well as benefits to patients. And in 2020, the Centers for Disease Control and Prevention (CDC) announced a partnership that aims to develop a national framework for medical-dental integration.
