Enter your email to receive the CareQuest newsletter:
Medicaid Adult Dental Coverage Checker
Identify Areas to Strengthen Adult Dental Benefits
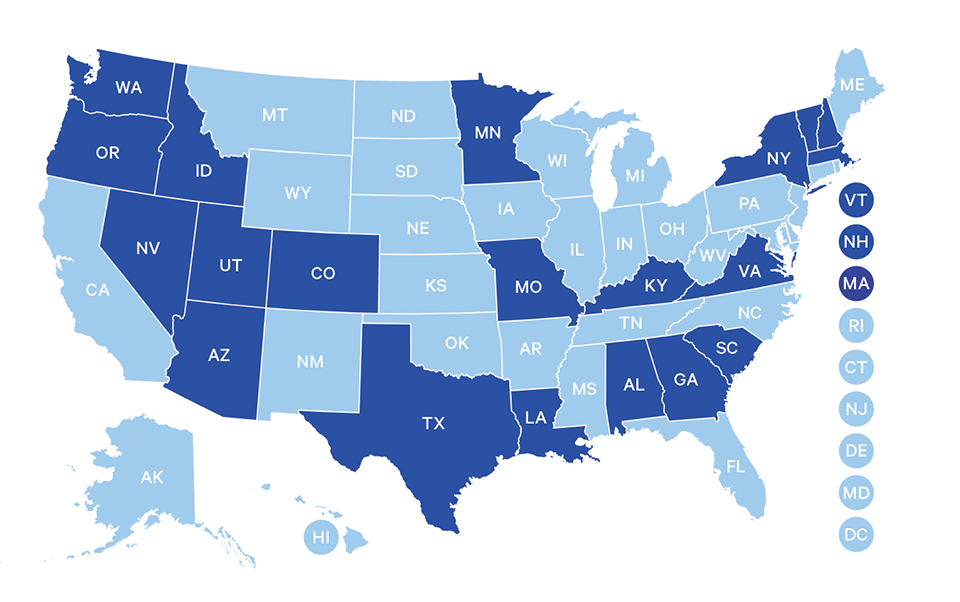
The Medicaid Adult Dental Coverage Checker is an interactive tool for policymakers, administrators, and advocates to better understand where a given state’s Medicaid adult dental benefits package falls on a continuum from no dental benefits to extensive benefits, helping identify areas for improvement. It looks at coverage of specific procedures and services, including allowed frequency, in eight service categories.
The Coverage Checker displays results that were self-reported by state Medicaid dental programs in a survey conducted in the spring of 2024. The data represent a snapshot in time and are reflective of the benefit package in place as of December 31, 2023. It’s important to note that several states have implemented new and expanded benefits for all adults in early 2024, which are not captured in the Checker. Please continue reading below for more information.
The survey mentioned above was developed in partnership with the American Dental Association Health Policy Institute (ADA HPI), Center for Health Care Strategies (CHCS), CareQuest Institute, and an advisory committee of experts in oral health care and state policy (please see below for further information).
Data visualization by Madison Vinson, MSHI and Adrianna Sonnek, MPH, Analytics & Data Insights, CareQuest Institute
States That Have Improved Medicaid Adult Dental Benefits in 2024
Connecticut
Effective January 1, 2024, Connecticut Medicaid covers certain periodontal services for qualifying “HUSKY” and “Covered CT” members.
Adults 21 years and older qualify when they have both of the following:
- Treatable periodontal disease determined by assessment performed by an oral health provider and reviewed during the prior authorization process, and
- A diagnosis of at least one of the medical conditions listed in the FAQ evidenced by medical claim history (the member has to have a diagnosis of condition in their medical claim history).
Prior authorization for treatment is required. Historically, Connecticut has not covered periodontal services at all for adults.
Kansas
In Kansas, dental exam and cleaning coverage is anticipated to begin around July 1, 2024. This expansion builds on incremental improvements to strengthen the adult dental program over the past several years.
In the spring of 2024, the Legislature approved additional funding to cover an expansion of its benefit package to include examinations and cleanings —
Making these preventive services part of the state Medicaid dental benefit will allow for more predictability to consumers and providers and is expected to increase adult access to dental care.
Minnesota
Effective January 1, 2024, Minnesota provides dental benefits based on medical necessity to all Medicaid enrolled adults.
In May 2023, the Health and Human Services omnibus bill was signed into law. Among other provisions, this legislation requires the state to provide dental benefits based on medical necessity to all Medicaid enrolled adults, regardless of age or pregnancy status.
In 2009, Medicaid dental benefits for adults were significantly reduced due to budget cuts. Minnesota has since had two different dental benefit sets for Medicaid enrollees, including a benefit set for pregnant adults and children and a benefit set for nonpregnant adults. While pregnant adults and children under the age of 21 received extensive benefits, many adult enrollees were not covered for these same services until this year.
You can find a full listing of covered services and frequency limitations within the Minnesota Department of Human Services Provider Manual.
Nebraska
As reflected in the Coverage Checker, Nebraska covers a wide range of dental services for its Medicaid adult beneficiaries, but adult beneficiaries had been limited to an annual benefit maximum of $750. Many have found this annual benefit maximum to be insufficient to meet their needs and a barrier to completing treatment plans in a timely manner. Effective January 1, 2024, Nebraska eliminated its annual dollar limit on dental benefits.
In January 2024, the Nebraska Department of Health and Human Services filed a Medicaid State Plan Amendment (SPA) with the Centers for Medicare and Medicaid Services (CMS). The SPA proposed to eliminate the $750-per-year adult dental benefit limit to allow licensed public health dental hygienists to provide certain dental services and to better align language in the State Plan with state regulations.
CMS approved this amendment in February 2024 with an effective date of January 1, 2024.
Utah
Utah is in the midst of making updates to its Medicaid adult dental benefit, though the timeline for implementation is unclear.
Signed into law in March 2023, Senate Bill 19 requires the state to seek approval from CMS to expand dental coverage to all adult Medicaid beneficiaries.
Currently coverage of diagnostic, preventive, endodontic, prosthodontic, and extraction services is provided to adults with disabilities and/or visual impairments, those aged 65 and older, those enrolled in Targeted Adult Medicaid receiving treatment for substance use disorder, and those who are pregnant or in the 12-month postpartum period.
If Utah’s waiver is approved by CMS, the above-mentioned coverage will be extended to all Medicaid adult beneficiaries. At the time of this writing, Utah’s waiver is under review and the timeline for implementation of the new benefit remains to be determined.
West Virginia
In the spring of 2024, Governor Jim Justice signed House Bill 4933 into law. This legislation changes the state’s annual benefit maximum, or cap on per member per year dental spending, from $1,000 per year to $2,000 over two years. This change is intended to allow beneficiaries to receive both an upper and lower set of dentures at the same time. This builds on recent improvements to West Virginia’s adult dental benefit implemented in 2021.
The change to the annual benefit maximum will take effect July 1, 2024.
Tools for Oral Health Advocates
How States Are Using the Coverage Checker
Strengthening Connecticut Medicaid Adult Dental Benefits
Donna Balaski, DMD, manager of medical care administration for the Connecticut Department of Social Services, discusses the importance of periodontal coverage for adults on Medicaid, and how they used the Coverage Checker to improve benefits in Connecticut.
How West Virginia Is Using the Medicaid Adult Dental Coverage Checker
Jason Roush, DDS, West Virginia state dental director, says the Medicaid Coverage Checker is extremely useful for state leaders to see what bordering states are covering, and it’s helpful for oral health advocates and supporters. The Coverage Checker doesn’t just provide numbers — it tells a story that oral health leaders can tell state lawmakers.
Maryland’s Successful Path to Securing Dental Coverage for Low-Income Adults
The tragic death of 12-year-old Deamonte Driver from an untreated tooth infection first compelled advocates in Maryland to take up the fight to expand dental coverage to low-income children in 2007. As they made meaningful advances in dental coverage for children, the Maryland Dental Action Coalition then turned its attention to expanding dental coverage for adults on Medicaid.
Featured News & Resources
Acknowledging Our Partners
The Rubric for Assessing Extensiveness of State Medicaid Adult Dental Benefits was developed in partnership with a core group and an advisory committee of experts in the field. After significant expansion and restoration of Medicaid adult dental benefits in several states several years ago, CareQuest Institute and the ADA Health Policy Institute collaborated to update the ADA’s classification of states.
Buoyed by these policy wins, CareQuest Institute shared that new round of classifications with grantees and partners and realized there was an appetite to form a larger workgroup. That workgroup quickly decided the oral health community would benefit from a new assessment tool, something that would move the industry beyond simply counting the number of procedures covered. The Coverage Checker is the output of that years long effort.
Core Group Organizations

Advisory Committee Members
Stacey Auger, MPH, Policy Consultant, CareQuest Institute for Oral Health
Donna Balaski, DMD, Healthcare Administration Management, State of Connecticut, Department of Social Services Division of Health Services
Melissa Burroughs, Director of Public Policy, CareQuest Institute for Oral Health
Stacey Chazin, MPH, MSODL, Principal, Chazin Consulting
Dora Fisher, Formerly Director of Older Adult Programs, Oral Health America
Chelsea Fosse, DMD, MPH, Director of Research and Policy Center, American Academy of Pediatric Dentistry
Steven Geiermann, DDS, Retired, Senior Manager, Access, Community Oral Health Infrastructure and Capacity, American Dental Association Council on Advocacy for Access and Prevention
Tracy Gilman, CDA, MSM, Formerly Regional Director, MassHealth Contract at DentaQuest
Carrie Hanlon, MPP, Formerly Project Director, National Academy of State Health Policy
Robert Isman, DDS, MPH, Formerly Dental Program Consultant, California Department of Health Care Services
Michael Monopoli, DMD, MPH, MS, FACD, FICD, Formerly Vice President for Grant Strategy, CareQuest Institute for Oral Health
Bianca Rogers, Formerly Advocacy Coordinator, Oral Health America
Andrew Snyder, MPA, Formerly Project Director, National Academy of State Health Policy
Madeline Steward, MPH, Program Officer, Center for Health Care Strategies
Nicole Taylor, MPH, Director for Population and Public Health, National Academy for State Health Policy
Marko Vujicic, PhD, Chief Economist and Vice President, American Dental Association Health Policy Institute
Cassandra Yarbrough, MPP, Formerly Lead Public Policy Analyst, American Dental Association Health Policy Institute