Enter your email to receive the CareQuest newsletter:
March 18, 2025
For Jessica Robertson, DMD, relocating from Southern California to rural Arizona has taken some adjusting.
“Moving to a small town was quite different,” she says, “not having a mall just around the corner or the amusement park an hour away.”
Some of the clinics where she provides care are even farther.

Robertson is a board-certified pediatric dentist at Around the Mountain Pediatric Dentistry, which has three clinics in rural Arizona: Cottonwood, Pinetop-Lakeside, and Flagstaff. She is also Chair of the ADA Council on Advocacy for Access and Prevention and served as an expert panelist on CareQuest Institute’s recent webinar “Starting Strong: The Importance of the Age One Dental Visit.” Robertson and Nick Rogers, DDS, shared why dental visits at age 1 are critical to promoting oral health and minimizing the risk of early childhood caries.
During the webinar, Robertson mentioned that she drives up to three hours to get to her Pinetop-Lakeside clinic. The commute is even longer for some of her patients.

“We have some patients who are local — and some who drive from four to six hours one way,” she says.
This distance from places like dental offices and grocery stores makes it challenging for patients in rural Arizona to have good oral health.
Patients are “only coming into town once a month to get their groceries,” Robertson explains. “So, their perishables will be done and over with within the first two weeks. And then the next two weeks are just ultra-processed foods, which are high in sugar and salt.”
And the consequences of that option-free diet are apparent in the mouths of the children she sees daily.
“I wish I could see every kid by age 1, but there are still a lot of kids at age 1 who are getting a lot of cavities,” she says.

A joint study in 2022 by CareQuest Institute, Arizona Oral Health Coalition, and Children’s Action Alliance found that despite recommendations that children see a dentist by their first birthday, less than 1% of Medicaid-enrolled children had a dental claim before the age of 1. The authors also wrote, “Arizona struggles with recruiting and sustaining dentists, particularly in rural and low-income areas.”
Below, Robertson goes into greater depth about the barriers patients in rural Arizona face in accessing oral health care, why the area struggles to gain and retain providers, and what oral health providers can do to improve access for their patients.
Can you tell us about your patient population and what oral health problems they have?
We are probably 60/40 in terms of Medicaid to private insurance fee-for-service. We also see a lot of pediatric patients from the reservation as well.
We’re seeing a lot of kids at 5 and 6 years old, and it’s not fillings that we’re doing — it’s crowns and extractions and spacers.
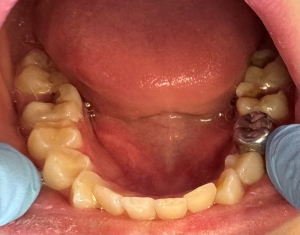
says, "and it’s not fillings that we’re doing — it’s crowns and
extractions and spacers."
We're doing a lot of sedations. We’re doing a lot of general anesthesia appointments. We’re doing a lot of silver diamine fluoride (SDF) on those individuals because we’re not going to see them under general anesthesia or sedation until they’re at least 2 years old and 25 pounds. With SDF, we’ve been able to push it to 3 years old and 30 pounds. Seeing a child closer to 3 ensures all the baby teeth have come in and decreases the chances of additional sedations in the future.
What does a typical day look like for you?
From my home in Cottonwood, it’s a three-hour drive to the Lakeside clinic. I go once a month because there are four practitioners, and we each cover a week.
I see about 35 to 45 patients a day. I know there are other practices that see close to 100 patients a day, but our patients are coming from far away. We want to make sure we have time for them. Also, in the state of Arizona, you have certain parameters with Medicaid that if a patient is in pain and it’s an emergency (potentially life-threatening), you need to see them that day. If they’re in pain but it’s not an emergent, we must see them within 24–48 hours.
What is one of the biggest barriers your patients face?
Food deserts. How do you tell your patients who are coming into town to shop for groceries once a month that sugary cereal is not a good idea? “Let’s get some eggs.” Well, the cost of eggs is $10 a dozen now. How do you keep those fresh? Maybe they could get chickens, but it’s hard to keep those chickens fed in a desert.
In the Native American population, a major health risk is diabetes, and you can understand the challenges they face when you’re driving across the reservation and how remote everything is. We’ve had to drive to Durango, which from Flagstaff is about a five-hour drive, and we drive right through the reservation. I remember stopping at one of the fast-food restaurants to grab something to eat. A popular menu item? Hot Cheetos with Kool-Aid powder on top. When processed foods that are high in sugar are among the only choices, it’s no surprise that diabetes and dental disease rates are so high.
What other barriers to accessing care do pediatric patients and their families face?
You sometimes have grandparents — and even great-grandparents — raising kids because the parents may have a drug addiction or are in prison. The parents are just not present. So, we’re having older, mature folks taking care of young kids who are energetic. And then they’re just trying to do their best and feed them on a very limited diet because they are out in remote areas.
Another huge barrier for some of our individuals who are not on Arizona Health Care Cost Containment System (AHCCCS), the state’s Medicaid program, or Medicaid is the cost of care, and families have a hard time coming up with the funds.
Why aren’t providers moving to the area?
A few reasons:
- Flagstaff is an expensive area to live in because there are a lot of second homes in Flagstaff and Lakeside-Pinetop. So, you’re having individuals who are buying up all these properties and driving up the prices, and then the local individuals can’t afford to live there. In other locations, like Cottonwood and Show Low, it shouldn’t be as expensive, but it is.
- I also think the debt load is a barrier for students these days because it’s so high. They just don’t think they can afford living there or purchasing a practice. But it is very doable. It’s just sitting down with them and their situation and doing the numbers for them.
- Sometimes their spouse does not want to live in a small community. You could have a successful practice, but if the spouse isn’t willing to be in a small town, it’s just not going to work.
- We also don't have a mall in Lakeside-Pinetop or in Cottonwood. So, when somebody’s looking for a place and they can only shop at Walmart, that could be a barrier.
So, what can we do about this? As Chair of the ADA Council on Advocacy for Access and Prevention, what are your goals to improve access to oral health care?
This year, it has been difficult to move the needle forward because we’re getting so many challenges about fluoride. You can only spread yourself so thin, and a lot of resources are going toward education of the importance of fluoride. Without fluoride in drinking water, you’re affecting individuals who are at higher caries risk — like these kids in rural areas— who should be on fluoridated water but can’t be because they’re in food deserts with no access to clean drinking water. They are coming into town to get their five-gallon water jugs and then taking them back. If they had access to fluoridated water in town, they would have some protection. Unfortunately, they are not, and we are fighting an uphill battle. They’re also buying drinks like juice and soda at the store that don’t expire, instead of the milk or just regular water, because buying water is still expensive. We want to target and educate those who can’t get access to dental care.

only choices," Robertson says, "it’s no surprise that diabetes
and dental disease rates are so high."
We are also trying to reduce sugar intake in the US. Sugar is a toxin, and we have too much of it. The entryway to the rest of the body is the mouth, and so one of the first things that you’re going to see in individuals with high sugar intake is cavities, and then down the road, they are going to develop diabetes. Then they're going to see heart issues and brain issues because they're going to start to develop type 3 diabetes with neurocognitive effects. And it all starts in the mouth, and if we can stop the infection and inflammation in the mouth, then we can help the whole entire body.
What can any oral health provider, no matter where they live, do today to help their patients?
We need to continue teaching it forward that oral health is the start of a healthy lifestyle and a healthy life. We need to be that investigative reporter to figure out why are you, as an individual, getting all these cavities? Is it because of your diet? Is it because you have acid reflux? Is it because you have huge tonsils and you’re a mouth breather? It’s all related. We get to practice a whole-practitioner approach in Northern Arizona because we don’t always have those primary care practitioners. We need to make sure families are aware that oral health affects the whole body.