2024 CareQuest Institute Impact Report
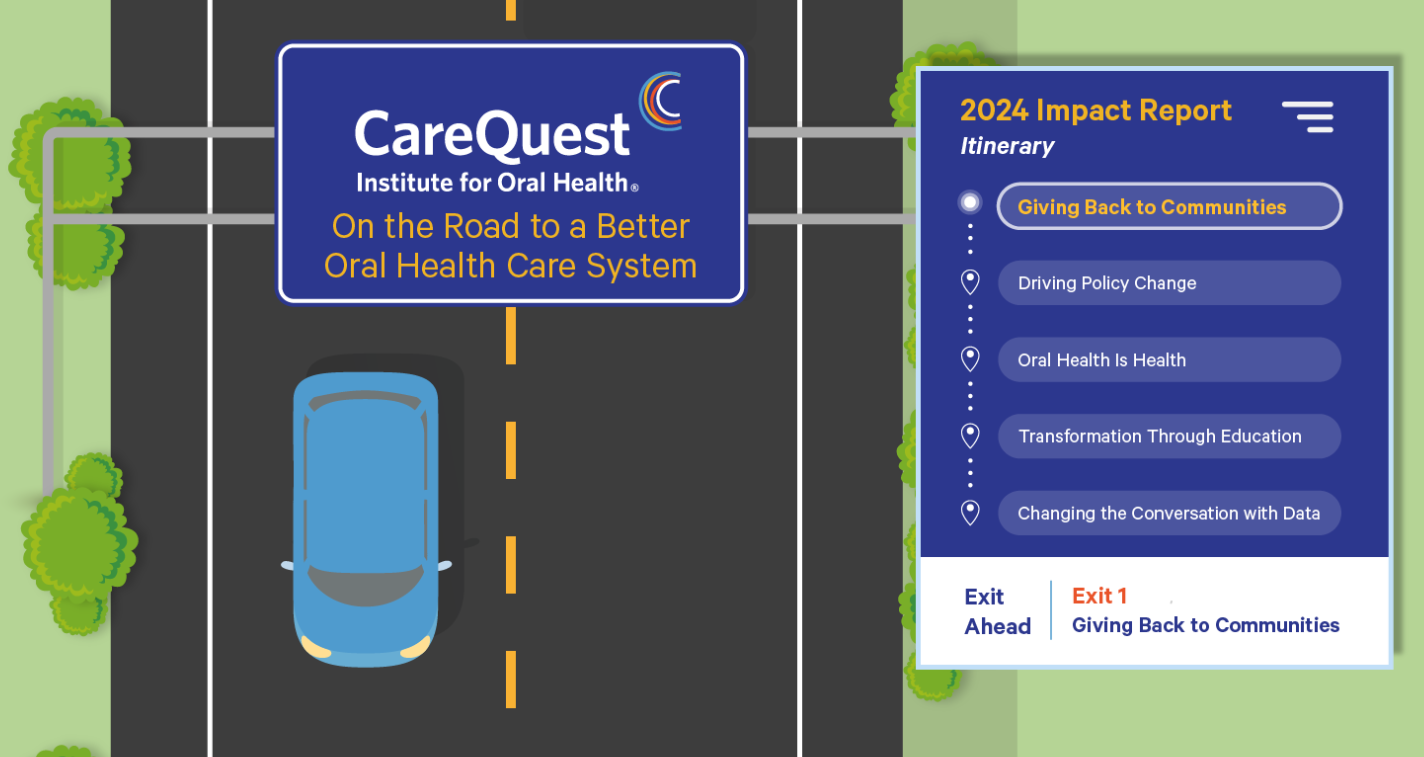
As 2024 comes to an end, the road to creating a better oral health care system continues. Yes, we saw roadblocks and detours, but we also made tremendous progress as a community committed to change.
There were several memorable stops and milestones along the way:
- This year, CareQuest Institute joined other oral health leaders and organizations in Washington, DC, to testify about how oral health care is out of reach for millions of people who live in the US.
- CareQuest Institute provided more than $12 million in funding to organizations who are trying to improve oral health care access to underserved populations — like children, rural communities, and veterans.
- The Institute also delivered more than 20,000 hours of education — giving dental and medical professionals the knowledge and skills they need to improve their individual practices and contribute to the broader transformation of our oral health care system.
Within all that work, 11 quotes from CareQuest Institute and CareQuest Innovation Partners — a for-profit subsidiary of CareQuest Institute — stood out as the most memorable. Below, we invite you to share in some of the successes and examine some of the issues that need attention in 2025.
1. “The more awareness we have, the more likely we can break down barriers to care, provide more inclusive care, and create a more trusting environment.” — Robert MacArthur, DMD, dentist, Boston Health Care for the Homeless Program
Robert MacArthur identifies as a cisgender gay white male and understands the value of having a dentist you can trust. But even though he’s a member of the LGBTQIA+ community, he says he still has a lot he can learn about creating a space where patients — especially from underserved communities — feel welcome. MacArthur attended the CareQuest Institute webinar “LGBTQIA+ Oral Health: Creating Inclusive Environments,” where he learned about inclusive language, proper pronoun usage, and different forms of gender expression.
2. “My dental care experience turned out to be much more expensive, invasive, and painful than it needed to be. And it was because while my doctors had recognized that oral health is part of the overall larger picture, my insurance didn’t.” — Paul Gibbs, volunteer member, Utah Consumer Health Coalition
In 2009, Gibbs needed a kidney transplant, but his doctors said first he needed to get a dental exam — which was not covered by Medicare or Medicaid. Gibbs was able to raise the funds for the exam through donations from friends and family, but his dentist found other issues Gibbs would have to address over the next few years after the transplant. By the time he got dental insurance, some of his teeth had disintegrated and some had to be extracted.Gibbs is now part of the Utah Health Policy Project’s Oral Health Consumer Coalition Committee, where he and other volunteers share their stories with legislators, hoping to improve oral health in their state.
3.“Far too many people in this country have discovered that oral health care is too expensive and out of reach. Yet this issue has been really on the back burner when it comes to policy conversations and the political commitment to addressing it.” — Melissa Burroughs, Director of Public Policy, CareQuest Institute
The USA Today article “Dental Coverage for Seniors Is Wildly Popular. Why Don’t Candidates Discuss It?” references a CareQuest Institute poll result that showed that about 9 in 10 voters support adding a dental benefit to Medicare. Adding dental coverage to Medicare ranked the second-most important topic in that poll, ahead of abortion rights and the future of the Affordable Care Act. Despite that, neither Vice President Kamala Harris or former and future President Donald Trump mentioned extending dental coverage in their platforms or major speeches leading up to the 2024 election.
4. “Through the SMILE Health validation studies . . . we now understand other avenues and opportunities in which we can provide oral health and nutrition information in a way that is accessible and reaches low-income communities.” — Shireen Abdullah, MBA, PMP, founder and CEO, Yumlish
Six oral health startups are now graduates of CareQuest Innovation Partners’ 2024 SMILE Health Cohort. SMILE Health, currently in its third year, is a 12-week semivirtual program that connects diverse innovators with a network of mission-aligned industry partners who help advance their solutions and road maps, in partnership with MATTER. As part of the 2024 program, startups receive a $10,000 stipend, take part in data-driven validation studies, receive mentorship, and participate in curriculum and networking.
5. “We’d get local anesthetic and two aspirin. After we left, we couldn’t have any more than two aspirin. And of course, that was kind of traumatic. I’ve probably had about four extractions while I was incarcerated.” — K. C. Uber, Oral Health Care Advocate
According to a CareQuest Institute Report, Oral Health in Incarcerated People, 50% of incarcerated individuals reported having a dental problem during the time they were imprisoned. Care for those patients typically means tooth extractions. For Uber, that’s the oral health care he received while incarcerated. Uber is now more than $11,000 in debt to pay for the implants that improved his oral health. He makes too much to qualify for Medicaid, and his insurance only covered cleanings.
6. “This is an issue that is not talked about anywhere nearly enough.” — Senator Bernie Sanders (I-VT), Chair, Senate Committee on Health, Education, Labor, and Pensions
In May, Myechia Minter-Jordan, MD, MBA, senior advisor to CareQuest Institute, testified on a panel of medical and dental professionals before the Senate Committee on Health Education, Labor, and Pensions. The hearing was in response to millions of people in the US struggling to get access to the oral health care they need — most often because they cannot afford it.Sanders introduced the Comprehensive Dental Reform Act of 2024 to try to expand Medicare, Medicaid, and Veterans Health Administration benefits to provide comprehensive coverage to seniors, veterans, and low-income families.
7. “I was in a crosswalk and struck by a bus. With dental, you’ll go to the emergency room, and they’ll treat anything but your teeth. And your teeth can be hanging, and they will give you antibiotics and tell you, ‘Go to a dentist.’ The only thing they will do for emergency dental is pull your teeth, but then I’d be walking around with no three front teeth. This isn’t appearance, this is health. Teeth are your health.” — Janessa, insured through Arizona Medicaid
Janessa is one of many people in the state who have a story about barriers to accessing oral health care. She is insured through Arizona Medicaid, but the state’s adult dental benefits only cover emergencies and are capped at $1,000, with very few exceptions. The Arizona Oral Health Coalition (AZOHC), with the support of grants from CareQuest Institute, is working to show legislators in the state the importance of oral health, its relationship to overall health, and the need for a comprehensive benefit.
8. “I appreciate all the ideas [from] the variety of presenters that I have seen and appreciate the online accessibility, especially living in a rural area where in the past I had to pack/drive/hotel for 3 days to take classes, so the low cost and convenience is amazing.” — Anne Premont, RDH, MS, MA, geriatric fellow
Premont is just one of thousands who attended CareQuest Institute webinars in 2024. Topics included oral health and pregnancy, new patient shielding recommendations, and oral health and cannabis. The Institute also offers self-paced courses featuring leading experts from across the oral health care field.
9. “There is such a pride in being able to do something that nobody else can do in dentistry. We really feel responsible to dentistry at large to make sure that things are done correctly because we know we’re in the spotlight.” — Bill Milner, DDS, MPH, founder, Access Dental Care
Access Dental Care, a nonprofit organization in North Carolina, participated in CareQuest Institute’s Community Oral Health Transformation (COrHT) Initiative in 2023. Through collaboration and networking, COrHT enabled teams to share insights and experiences to support each other. Milner was a peer mentor to other clinics since Access Dental Care had been providing care for special populations and using teledentistry for years prior to joining the initiative. Work with the Institute also helped Access Dental Care record value-based services that the organization hasn’t always had a way to track.
10. “We really wanted to promote the one-stop-shop, under-one-roof, collaborative care with the medical providers and really dig into why they weren’t seeking dental care at all or were going elsewhere.” — Rebecca Cornille, DDS, chief dental officer, Vista Community Clinic (VCC)
VCC, a Federally Qualified Health Center (FQHC) in southern California, was looking for a way to get pediatric medical patients to also go to their dental department. The FQHC had hired an integration coordinator for patients with diabetes in 2021, and Cornille says that inspired the idea of hiring an integration coordinator for their pediatric patients. VCC didn’t have the budget for the position, so it applied for — and received — a $125,000 CareQuest Institute of Oral Health grant as part of the Institute’s Community and Care Transformation initiative. Cornille says she’s hopeful the integration coordinator proves to be a financially sustainable and recognized position within the care team.
11. “It’s our intention to invest in communities that have been historically marginalized that haven’t had a seat at the table.” — Trenae Simpson, MBA, grants and programs director, CareQuest Institute
People who live in Connecticut, like many who live in the US, struggle with equal access to oral health care. In this video, oral health advocates, many at organizations funded by CareQuest Institute grants — like the Ministerial Health Fellowship, the Connecticut Oral Health Initiative (COHI), and the Connecticut Department of Social Services — explain how they work closely with the community to improve oral health and overall quality of life.
