Enter your email to receive the CareQuest newsletter:
April 11, 2025
Uncertainty? Yes, plenty of that. Apprehension? A bit. Anxiety? There was some of that too. None of those words, though, sum up the mood, feeling, and spirit of the 2025 National Oral Health Conference (NOHC).
The word that does? Resilience.

talking to people at CareQuest Institute booth
“Some people are more optimistic in times of change,” said Lyubov Slashcheva, DDS, MS, DABDPH, FABSCD, Research Director at Apple Tree Dental in Minnesota. “Like one of my policy colleagues, Dr. John Pournoor, says, ‘Never let a good crisis go to waste.’”
More than 650 optimistic oral health stakeholders — providers, policymakers, researchers, payers, educators, and students — spent a few days in Orlando earlier this week to share lessons about work they and their colleagues are doing to improve the oral health system in the US. The current and potential crises for the industry — the elimination of the Centers for Disease Control and Prevention’s (CDC) Division of Oral Health and the potential cuts to programs like Medicaid — were top of mind for many, as expected. Some attendees talked with frustration about canceled grants; others talked about feeling lucky to be unscathed. Together, though, a spirit of gratitude and a desire to help permeated the conference space. The dynamic presentations, the lightbulb moments of connection, and the stories and examples of progress emerged as the lasting takeaways.
“The mood?” Slashcheva thought for a moment before answering. “Resolute.”

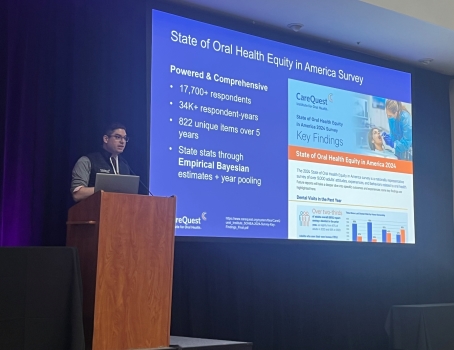
presenting at NOHC
Session Highlights: Seeking Innovations in Oral Health
The work of “finding innovations in oral health,” the theme of the conference, was on display on Monday and Tuesday, with nearly 40 educational presentations and a collection of roundtable discussions — several of which featured thought leaders from CareQuest Institute. They ran the gamut from incorporating oral health education into soccer programming and teledentistry in schools, to community water fluoridation updates and accommodating neurodivergent conditions in oral health. In the latter presentation, CareQuest Institute’s Lisa Heaton, PhD, and Josefine Ortiz Wolfe, PhD, MBA, MPH, RDH, shared a mix of research and personal stories that captivated a roomful of more than 80 learners on Monday morning.
“When we think about neurodivergence in the dental field, it’s important to address it because we want to provide the best care possible,” Ortiz Wolfe said. “Developing consistent provider-patient relationships is probably the most important thing of all because of the trust that builds.”
Heaton, a clinical psychologist by training, went a step further, sharing a practical piece of advice about trust-building: “Normalize actions as a way to help people advocate for themselves. Say things like ‘Lots of people like to use those dark glasses, or not everyone likes that feeling.' Showing you’re willing to talk about those things will make patients more comfortable."
In “Developing a Culture of Patient Safety in Dentistry and Why It Matters,” Clifford G. Lisman, DMD, MS, FACD, FAAPD, MBA, and Becky Parnian, DHSC, MPH, RDH, CDA, discussed the pillars of creating a culture of safety in dentistry on Monday afternoon.
“I shared errors I have made in my career,” Lisman said. “My motivation is I don’t want to see it ever happen again. I would encourage you to be open and transparent. It doesn’t diminish you; it elevates you. Transparency and humility go a long way.”
Parnian shared data from a survey of New Jersey dental professionals about the knowledge of and attitudes toward patient safety. She helped uncover several recommendations with her research:

white paper at NOHC
- Stronger safety policies
- Streamlined reporting guidelines
- Improved communication
- Mandatory training
- Simplified reporting system
In a very popular session on Monday afternoon called “10,000 People Turn 65 Every Day: What Oral Health Policies Are Needed?” speakers discussed the applicability of the Association of State and Territorial Dental Directors’ Health Aging Committee workgroup’s policy recommendations. Why are older adults at greater risk? The experts highlighted the use of medications that lead to a reduction in saliva flow, reduced efficacy of oral hygiene due to dexterity and cognitive changes, and greater exposure of root surfaces. Deborah Jacobi, RDH, MA, of Apple Tree Dental shared some of her organization’s work in long-term care settings that have been beneficial:
- On-site collaborations with nurses, physical and occupational therapists, and other team members
- Care planning with nursing staff, including writing daily mouth-care plans
- Admission screenings and completing the oral and nutritional sections of the minimum data set
- Physician consultations and coordinated care planning
In Tuesday’s popular keynote, “The Invisible Population: Oral Health Care in US Correctional Facilities,” the speakers helped attendees understand the correctional system and the gaps in the oral health needs of the population. Morton K. Rosenberg, DDS, homed in on the levels of dental disease for incarcerated individuals:
- Not much different than what is seen in low-income/medically indigent communities
- Majority of patients did not have access to oral health and utilized emergency departments
- More likelihood of drug abuse
- Higher incidence of oral maxillofacial trauma
“The most important thing we can do in the prison system is to treat today’s patient today,” he said. “Don’t kick the can down the road. Nothing good happens from that.”

Three Topics Took Center Stage
The sessions at NOHC covered multiple aspects and angles of oral health innovation. Here are three that rose to the top:
Integration continues to gain momentum. Connecting mental health and oral health. The role of school nurses in facilitating follow-up dental care. Integrating oral health into long-term care. Vaccinations in dental clinics. There were myriad ideas and learnings related to integrating oral health into other aspects of health care to improve care for patients.
Special populations need time and attention. From “10,000 People Turn 65 Every Day: What Oral Health Policies Are Needed?” to “The Invisible Population: Oral Health Care in US Correctional Facilities,” the needs of unique populations were on center stage. Ortiz Wolfe, in her presentation on neurodivergence, noted that the focus on special populations can help with all patients. “When we have people who are neurodivergent in our space, it makes us better providers, better oral health teams,” she said.
Data is a key that can unlock many doors. On Tuesday afternoon, CareQuest Institute’s John O’Malley, MHI, MS, unveiled the updated National Oral Health Data Portal, an interactive website designed to help public health stakeholders and the public find the information they need and want about the oral health system. The new portal highlights expanded capabilities, like allowing people to compare measures across sociodemographics and social determinants of health. The beta version is live, O’Malley announced to the full conference room, and there’s a full launch planned for later this year.
Said simply, it’s all the oral health data you want in one place.
“We found a way to take all different types of measures and all different types of scales and combine them into one spreadsheet,” O’Malley said, noting that enhancements are ongoing. “We are looking to integrate emergency department data and insurance claims. If you know of any data sets we should include, please let us know.”