By Stacey Auger, MPH, policy consultant, CareQuest Institute
In July, CareQuest Institute and a group of partners and advisors released the 2022 Medicaid Adult Dental Coverage Checker. This updated interactive tool allows policymakers, administrators, and advocates to understand where a state’s Medicaid adult dental benefits package falls on a continuum from no dental benefits to extensive benefits and to identify opportunities for improvement. With two sets of data (2020 and 2022) now captured in the Coverage Checker, we can see how the coverage landscape has changed over time.
That change, by and large, has been positive!
As the Coverage Checker shows, the period between 2020 and 2022 marked a significant expansion of Medicaid adult benefits across the country — one of the most significant in recent decades. 2023 has proven to be another big year for Medicaid adult dental benefits, and it looks as though even more positive movement is on tap for 2024. In 2024, we’ll add data reflecting coverage in place as of December 31, 2023, and we anticipate seeing great movement in many of the states you will read about below.
New Benefits Took Effect in 2023
The start of the new year ushered in significant benefit expansions in seven states:
- In January, Hawaii reinstated adult dental benefits that were eliminated in 2008. Maryland and Tennessee built upon benefit packages for specific groups of adults and implemented benefit packages for all adult beneficiaries.
- Kentucky, following the October 2022 announcement of Governor Andy Beshear’s new initiative to boost workforce participation by improving coverage of dental, vision, and hearing, expanded Medicaid adult dental benefits to include fillings, crowns, implants, and dentures.
- Michigan and New Hampshire added new benefits for all adult beneficiaries on April 1, 2023.
- In July, after a significant expansion of dental coverage in 2022, the Kansas legislature further expanded the benefit in 2023 to include full and partial dentures for all adult beneficiaries.
Access Granted: Number of Adults Who Benefit from Expanded Coverage in 2023
As a result of these expansions, more than 3.2 million adults in these seven states have gained access to new or expanded benefits in 2023. You can find more information on the benefits packages offered in these states.
Benefit Changes Coming in 2024
2023 also brought legislative victories in several additional states. As noted below, these improvements to Medicaid adult dental benefits are expected to take effect in 2024.
Connecticut: Thanks to the efforts of the Connecticut Oral Health Initiative (COHI) and its advocacy partners, the Connecticut Department of Social Service and Dr. Donna Balaski, and champions in the legislature, the new state budget includes funding for periodontal coverage for adults with certain medical conditions like diabetes.
Using COHI’s recent Medicaid Gap Analysis Report, which collected and analyzed Medicaid service utilization data, geographical information on the state’s provider network, and the experiences of Medicaid beneficiaries and providers, advocates showed that the lack of periodontal coverage within Medicaid was one of the most severe issues negatively affecting the oral health of adults in the state. The new periodontal coverage will take effect January 1, 2024, and advocacy efforts are afoot to make this benefit available to all adults in future years. Advocates will also pursue further improvements to the adult dental benefit in 2024, including the addition of a second dental cleaning, a reduction in the timeline for the replacement of prosthodontic appliances, and the modification of the annual benefit cap.
Minnesota: As part of the 2023 Health and Human Services omnibus bill signed in May, Minnesota will begin providing dental benefits in 2024 based on medical necessity, mirroring the benefit currently in place for pregnant women and children.
Multiyear advocacy efforts catalyzed this expansion of benefits. In 2021, periodontal services were restored as part of a broader legislative package that also increased state investment in Medicaid dental services. The Get to Yes coalition led these efforts, using stories, crafting effective messaging, and highlighting research and data. Bipartisan support in the state’s legislature and from the Department of Human Services bolstered the coalition’s work.
New York: In May 2023, a settlement was reached in Ciaramella v. McDonald, a federal class-action lawsuit brought against the New York State Department of Health in 2018 on behalf of Medicaid beneficiaries in New York who were denied coverage for medically necessary dental care. The settlement will bring expanded dental coverage of root canals, crowns, dental implants, and replacement dentures to roughly 5 million Medicaid beneficiaries in the state. The new rules are expected to take effect in early 2024.
Utah: Signed into law in March 2023, Senate Bill 19 requires the state to seek approval from the Centers for Medicare and Medicaid Services (CMS) to expand dental coverage to all adult Medicaid beneficiaries. This expansion follows previous incremental expansions for specific population groups: individuals with disabilities and/or visual impairments, those aged 65 and older, and those enrolled in Targeted Adult Medicaid (TAM) receiving treatment for substance use disorder. As with previous legislation, SB19 requires adults to receive their care through the University of Utah School of Dentistry (UUSOD) or its associates throughout the state. Also, similar to previous legislation, this bill does not contain a fiscal note as UUSOD pays the state’s portion to receive federal matching funds to provide care. At the time of this writing, Utah’s waiver application with CMS is pending.
Vermont: According to the 2022 Coverage Checker, Vermont was one of five states that increased annual dental services spending per member, also known as the annual benefit maximum (ABM), between 2020 and 2022. Most recently, Vermont Medicaid implemented three new changes that went into effect July 1, 2023:
1. The ABM was increased from $1,000 to $1,500 for adults who are not pregnant or in the postpartum period, or who are not in Department of Disabilities, Aging, and Independent Living Developmental Disability Services (DDS) Waiver Program or the Department of Mental Health Community Rehabilitation and Treatment (CRT) Waiver Program.
2. The ABM was eliminated for adults who are pregnant or postpartum as well as those in DDS and CRT Waiver Programs.
3. Coverage of medically necessary denture services was added for pregnant and postpartum adults as well as those adults in the DDS and CRT Waiver Programs.
The benefit improvements mentioned above are the result of years of relentless advocacy by countless local and state champions who are beneficiaries, caregivers, service providers, health professionals, academics, state officials, and lawmakers. For years, these advocates have worked to educate their communities about the importance of oral health and its connection to overall health, and to build public will and action for improving benefits and access to care.
Oral Health Will Remain a Top Priority in 2024 — and Beyond
Looking to build on their recent advocacy efforts and the momentum happening across the country, several states have already signaled that expanding Medicaid adult dental coverage is a top priority. To advance their work, advocates in these states are elevating community voices, relying on data, and turning policy recommendations into action.
Here’s a quick peek at some of the states we’re watching:
Arizona: Advocates have been making steady progress during the past several years, raising awareness of the need for an expanded adult benefit. During the 2023 legislative session, HB 2338 was filed to expand the existing dental benefit to include preventive services. While the bill successfully passed in committees in both chambers with strong bipartisan support, it did not receive funding in part of the state budget.
In 2024, the Arizona Oral Health Coalition (AZOHC), along with its legislative and policymaker champions, intends to file legislation and secure funding for an expanded benefit for all adults.
Leading up to the filing, AZOHC will continue to work with impacted communities and oral health stakeholders to grow the “oral health is essential” comprehensive advocacy campaign with a focus on elevating the need for a comprehensive adult dental benefit through continued lawmaker education, public engagement, and social media/media messaging. AZOHC will also use data from the recent CareQuest Institute report, “Spotlight on Arizona: Adult Use of Emergency Departments for Non-Traumatic Dental Conditions,” and a report from Grand Canyon Institute that explores some of the anticipated long-term cost savings to the overall health care system as the result of a comprehensive dental benefit.
“Because of advocacy efforts at the grassroots and legislative levels, we have seen oral health elevated at the State Capitol with broad bipartisan support,” says Brianna Miller, coordinator of the Arizona Oral Health Coalition. “State Representative, and conservative newcomer, Matt Gress, called the preventive dental bill, ‘fiscally conservative and morally right’ after hearing stories from Arizonans struggling to access oral health care, and gaining an understanding of the long-term health care cost savings associated with good oral health.”
Delaware: Championed by Senator Sarah McBride and Representative Melissa Minor-Brown, legislation was passed in April 2022 to create a Dental Care Access Task Force. The Task Force issued its final report in July 2023, in which it recommended the state expand its existing adult dental benefit by removing the annual benefit maximum and/or the emergency benefit maximum; increasing flexibility of the pre-authorization of the emergency benefit; and enhancing the benefit to cover high need services, including, but not limited to, crowns, root canals, and dentures. In the report’s opening message, Senator McBride noted that she is confident that the Task Force report represents a next step in the ongoing dialogue about how we can improve access to oral health in the state.
Florida: For adults in Florida, the state’s Medicaid program covers emergency dental services to alleviate pain, infection, or both, and procedures essential to prepare the mouth for dentures. Many non-emergency dental benefits are covered by Florida’s Medicaid Dental Managed Care Organizations as value-added or “expanded benefits.” These benefits, which vary by MCO, are not required under state law and are not written into the Florida Medicaid State Plan. Advocates have routinely called for clarity about what, if any, non-emergency dental benefits are provided through the Medicaid dental MCOs.
Florida Voices for Health is looking to change this. The organization is leading a statewide effort to expand Medicaid coverage of a wide range of dental benefits, including diagnostic, preventive, and restorative services. Providing this benefit will help Florida realize cost savings related to reduced emergency department (ED) use, chronic disease management, and a reduction in opioid prescribing.
Through story collection and dissemination, the hosting of roundtable conversations and community events, and creating opportunities for engagement, Florida Voices for Health seeks to bring impacted individuals, providers, stakeholders, and lawmakers into better conversation with one another to advance change.
“Our model focuses on sharing stories, data, and solutions in formats intentionally designed to meet lawmakers where they are,” says Scott Darius, executive director at Florida Voices for Health. “Consumers are at the heart of our model, and they ultimately drive which issues we elevate and which solutions we support.”
Kansas: Thanks to the steadfast advocacy of Oral Health Kansas and its partners across the state, incremental improvements to strengthen the adult dental program have been made year after year in Kansas. Most recently, dental benefits were expanded in 2022 and 2023 and now cover a wide range of services including fillings and crowns, periodontal care, silver diamine fluoride, full and partial dentures, and denture repairs.
Kansas is the only state to use a combination of Medicaid-provided benefits and value-added benefits (VAB) offered through the state’s three MCOs. Since 2013, when the state moved to a managed care model, all three MCOs that operate in Kansas have offered preventive dental services to adults through their VAB packages. Those VAB packages have evolved over the years, and now they each offer a benefit of $500 per year that covers exams and cleanings. The precise package offered by each MCO changes slightly every year.
Driven by the voices and concerns of Medicaid beneficiaries and providers, Oral Health Kansas will continue advocating for the inclusion of exams and cleanings in the Kansas Medicaid State Plan, which will ensure a comprehensive and secure package is available for Medicaid beneficiaries regardless of the VABs available each year, streamline the benefits package, and avoid confusion.
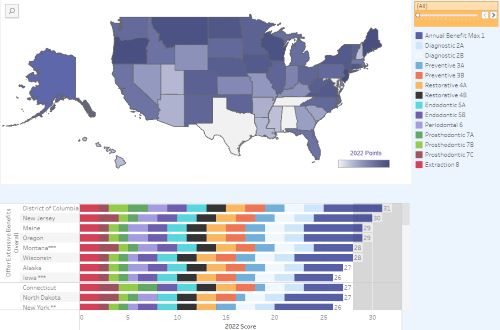
2022 Medicaid Adult Dental Coverage Checker
“Oral Health Kansas has worked hard to curate and collect data to complement the stories we hear in order to prove the oral health issues in our state are systemic,” says Tanya Dorf Brunner, executive director at Oral Health Kansas. “For so many years, legislators’ hesitancy to allocate funds for adult dental services has been due to the price tag associated with increased dental benefits, but by being able to show a positive offset in other medical expenses and emergency room visits we were able to gain support from legislators for an extended adult dental benefit. It was this collection of data, along with the real human stories, that showed legislators the need to invest in our state’s Medicaid dental program leading to legislative wins over the last five years.”
Nebraska: For the past several years, Nebraska Appleseed has been working to identify systemic oral health care issues and solutions that are community priorities, as well as building and maintaining relationships with impacted Nebraskans who can become powerful, long-term advocates. In 2024, the organization will deepen its oral health care advocacy by building off its Medicaid dental policy brief; participating in a legislative interim study focused on dental care; and monitoring the state’s removal of the Medicaid dental cap and the state’s transition to having multiple dental MCOs in the new year.
North Carolina: In March 2023, North Carolina passed Medicaid expansion legislation. The expansion will take effect on December 1, 2023, and is expected to cover an additional 600,000 North Carolinians. North Carolina Medicaid offers dental benefits to adult beneficiaries, and it is expected that these benefits will be extended to newly eligible adults. In the year ahead, we will monitor the implementation of Medicaid expansion in the state and what it means for beneficiaries accessing dental care.
Pennsylvania: In 2011, comprehensive dental benefits for adults were cut, eliminating reasonable access to covered emergency exams or services like gum disease treatment, crowns, root canals, and dentures. Since that time, advocates across the state, led by the Pennsylvania Coalition for Oral Health, have been calling for a restoration of benefits as well as several additional systems-based improvements.
At the time of this writing, advocates and legislative champions are pursuing companion bills HB1417 and SB955, which would reinstate all previously eliminated dental services, eliminate the existing Benefit Limit Exception (BLE process), and allow for additional services to be covered. Pennsylvania is in the midst of a two-year legislative cycle and we’ll be watching the progression of this important piece of legislation.
“With a new administration and two-year legislative session starting in 2023, Pennsylvania is primed for change,” says Helen Hawkey, executive director at the Pennsylvania Coalition for Oral Health. “Paramount to equitable access to oral health is the reinstatement of comprehensive benefits for adult Medicaid members. In 2011, benefits were cut for the state budget to save $42 million. Twelve years later, the consequences of this decision have compounded barriers for the most under-resourced Pennsylvanians. Recent projections from the state Medicaid office show the cost of restoring benefits is $176 million, demonstrating a significant increase because of the state’s neglect.”
How to Get Involved in Expanding Benefits
We’re excited to see oral health at the forefront and encouraged by the progress all stakeholders have made in recent years. It’s incredibly impressive. Still, work remains, and the weeks and months ahead will be busy ones for advocates and policymakers. If you share in our excitement and want to get involved in the advocacy to further improve Medicaid dental coverage for adults, you can:
1. Get involved with your statewide coalition! Check out any of the advocacy links throughout the post or reach out to us and we’ll help connect you.
2. Sign up for the CareQuest Institute newsletter to get the latest on dental benefit expansion and progress.
3. Explore the Medicaid Adult Dental Coverage Checker to see where your state’s benefits package falls on the continuum from no benefits to an extensive benefit.
4.Reach out to your elected officials to let them know you support dental benefits for all adults. Check out the “Tools for Oral Health Advocates” section on our website for more information and links to contact your state and federal legislators.
